See the expert for eyelid movement conditions in Nashville, TN.
Why Choose Sherman Aesthetic Center?
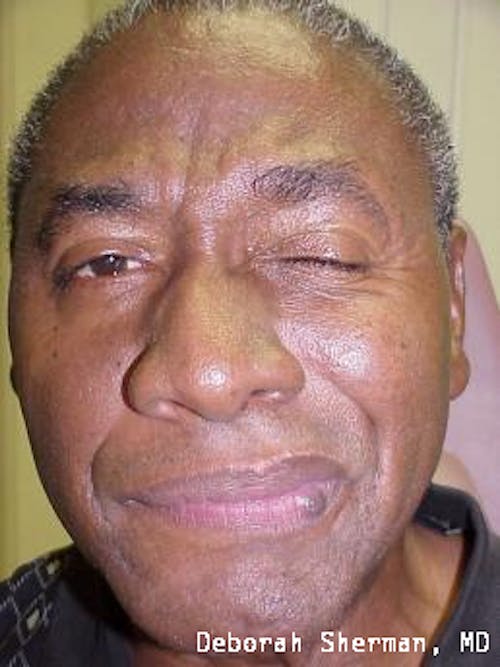
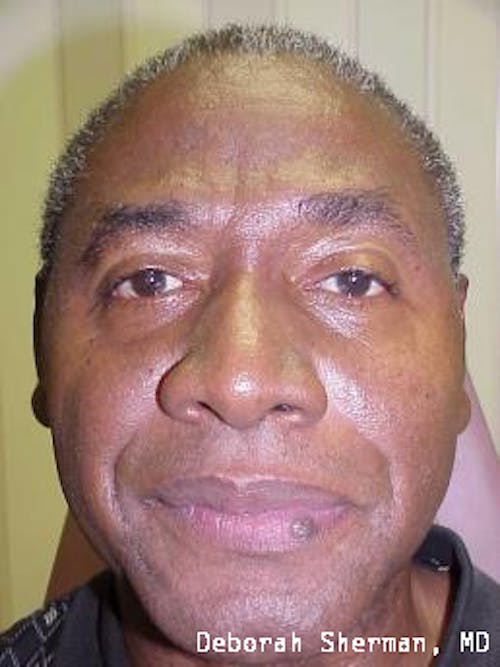
Sherman Aesthetic Center founder Dr. Deborah Sherman is a national and international trainer for BOTOX and has taught her master injector techniques extensively with other physicians in the US, as well as Russia and China. She has also been injecting Xeomin since its FDA approval in 2011. This level of experience and expertise in the injection technique makes Dr. Sherman a well-qualified specialist with the highest level of training in treating blepharospasm and hemifacial spasm. Dr. Sherman and Dr. Mark Melson of Sherman Aesthetic Center specialize in many different types of operations to help the rehabilitation of patients with facial nerve palsy. As board-certified ophthalmologists and fellowship-trained eye plastic surgeons, Dr. Sherman and Dr. Melson can evaluate and advise you on all available treatment options to reduce eyelid spasms and restore healthy eyelid movement and function.